As an herbalist for nearly 40 years now, I’ve learned a great deal about this controversial medicinal plant, but it was in my medical residency at Yale that I really saw the light. I worked with many patients who shared their experiences of getting relief from pain with Cannabis, to the extent that it allowed them to reduce their use of narcotics. This was before the opioid epidemic hit in full, but I saw it brewing. So I got permission to embark on a study into the use of cannabis for pain relief, which ultimately convinced me that it had enough scientific merit as a pain-relieving medicine to warrant inclusion in my textbook, Botanical Medicine for Women’s Health (yes, I actually wrote the textbook on women’s herbal medicine!), and to use as a medicine in my practice.
So if that time of the month and period pain gets you curled up in a ball, or stretched out on your sofa binge-watching Netflix hugged up with your best friend at the moment – your hot water bottle – have a read (or listen to the podcast). This may be an herbal medicine that you too will find fascinating, and perhaps one that brings you some relief when you need it.
Love to read? Enjoy the article below. Don’t have time? Click the player to listen.
Period Pain: What’s Going On?
Over your monthly menstrual cycle, under the influence of estrogen, your uterine lining (endometrium) naturally thickens into a nutrient-rich ‘bed.’ This lush lining will support pregnancy should a woman conceive. But if conception doesn’t occur, your body does the work of ‘Marie Kondo-ing’ out that lining. It does so with the help of a group of chemicals called prostaglandins, in this case inflammatory ones, that cause both the blood vessels in the uterine lining and the muscular uterus itself to contract. These prostaglandins also have additional effects: they increase overall inflammation and sensitivity to pain, and if that’s not enough to make you uncomfortable, they loosen our stools, too, which is why you may ache or have to go to the loo more before your period.
Half of all menstruating people experience somewhere from mild to debilitating period pain, technically referred to as dysmenorrhea. There are two types of dysmenorrhea:
Primary dysmenorrhea is what we think of as ‘typical’ menstrual cramps. It generally starts 1 to 2 days before your period begins and lasts for the first 1 to 3 days of bleeding. Having a minor amount of fullness in your pelvis, aching in your abdomen, lower back, or inner thighs, minor cramping, or some looser stools before your period is normal and natural. It’s caused by all of the normal physiologic changes I described above.
More than a little period pain, though, can be a sign that it’s time to look into the root causes, which may include underlying inflammation, hormonal imbalances (i.e., high estrogen levels), or being low in the nutrients that counterbalance prostaglandin-induced inflammation (i.e. Vitamin D, Essential Fatty Acids like DHA and EPA found in fish and fish oil) or that prevent cramping (i.e., calcium, magnesium) and which I discuss here, along with some of the holistic strategies that are effective for preventing and reversing period pain, including heat, specific yoga postures, calcium, magnesium, and ginger, among others.
Secondary dysmenorrhea is period pain due to an underlying or concurrent gynecologic condition – usually endometriosis, or adenomyosis. The pain, which as you know if you experience it, can be quite severe. It may begin earlier and last longer than with primary dysmenorrhea, and you may also have other symptoms, for example, pain with penetrative sex, bowel symptoms, or urinary symptoms, as well as chronic pelvic pain throughout the month. In an article and podcast here I talk about natural treatments for endometriosis, which also apply to adenomyosis.
However, you may still find that you need in-the-moment period pain relief, either while you’re getting to the root causes or for the occasional painful period.
The Problem With NSAIDs
The most common medication that women turn to for menstrual pain are the non-steroidal anti-inflammatory drugs (NSAIDs), particularly ibuprofen (i.e., Motrin® and Advil®). They work by inhibiting an enzyme, COX-2, involved in the production of those inflammatory prostaglandins I mentioned, and as a result they reduce cramping, inflammation, pain, and also heavy menstrual bleeding. All good things! Unfortunately they also inhibit COX-1, and this can result in the stomach and digestive symptoms so common when taking NSAIDs, like gas, bloating, and heartburn.
NSAIDs use also comes with a set of potential adverse effects including:
- Risk of stomach bleeding
- Increased heart attack risk, even when just used for a short time, and in those who do not have prior risk; the risk goes up with regular use, especially in those who do have heart disease risk factors (smoking, high blood pressure, high cholesterol, diabetes).
- Inhibition of ovulation and reduction in progesterone levels, which can undermine fertility,
For those with secondary amenorrhea, the pain may be severe enough to seek medication that is even stronger; 25% of women with endometriosis are prescribed a narcotic (opioid) – and as you likely know, this can be a dangerous road with high risk for addiction, side-effects, and even accidental overdose. The overdose risk for women with endometriosis is compounded by the fact that many physicians prescribe a benzodiazepine for concurrent use to treat anxiety, which increases overdose risk by 10 times! Few are informed of this risk.
While I do recommend NSAIDs for occasional use when needed to cope or function, I encourage my patients to avoid narcotics, and whenever possible, reach for natural alternatives.
Enter Cannabis: A Traditional Period Pain Relief Remedy
The medicinal use of Cannabis can be traced back thousands of years. According to my colleague and friend, Ethan Russo, MD, and co-author of Women and Cannabis: Medicine, Science and Sociology with Mary Lynn Mathre and Melanie Creagan Dreher, the use of Cannabis for relief from period pain dates back to ancient Egypt, where the Ebers Papyrus (1550 BCE) and other papyri indicate that women prepared an ‘oxymel’ with Cannabis and honey to be inserted vaginally. Vaginal suppositories and similar preparations are a common way that Cannabis was used historically.
An early pharmacy book, written circa 2737 BCE by the Chinese Emperor Shen Nung, references the use of Cannabis, and its use for menstrual pain is described in a Chinese text that dates back to 1596 BCE. References and artifacts of its use are also found in ancient Persian, Middle Eastern, Ayurvedic, and Semitic writings. It is thought that the plant was used in parts of Africa, and seeds brought to the americas (sic) by enslaved Africans.
The Royal We(ed)
Documentation of Cannabis’ effectiveness in relieving menstrual and pelvic pain continues throughout history, eventually appearing widely in the British and American medical literature of the 1800s. Cannabis even famously made its way into England’s royal court where, for 30 years, Queen Victoria’s physician, Sir J. Russell, provided her with monthly doses of Cannabis extract to treat her menstrual pain. He likely learned of its use through the writings of a 30-year old British doctor serving in India, W. B. O'Shaughnessy, who brought its use to the attention of European physicians around 1839, recorded indigenous use, and sent seeds back to England which were grown in Kew Gardens, after studying and being impressed by its over 1000-year traditional use in India. So taken was Russell with its effectiveness, based on his own 30 years of careful observations of its use in his clinical practice, that he wrote an article, published in 1890 in the medical journal The Lancet (which remains a leading medical journal today), describing Cannabis as one of the most valuable medicines we possess for dysmenorrhea, among other symptoms and conditions. The British Pharmaceutical Codex retained an indication for Cannabis for the treatment of dysmenorrhea until 1934.
A Role in US Medical History, Too
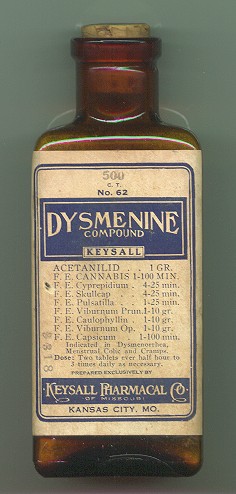
Cannabis extracts were commonly used for medicinal purposes and could be even be purchased at a pharmacy, without a prescription, into the early 1940s in the United States. A pharmaceutical for the treatment of dysmenorrhea, Dysmenine Compound, was produced in the US in the late nineteenth century by the Keysall Pharmacal Company. Its key ingredient? Cannabis.
Cannabis remained an official medication of the US Formulary, and wasn’t removed from the United States Pharmacopoeia until 1942. As a result, it fell out of use as a prescription by physicians, and political forces led it to be thought of as a drug with a lot of stigma associated even with personal use. Yet, for many, it remained a medicine of interest. As one example, in 1971, Solomon Snyder, a neuroscientist at John’s Hopkins University (a mentor to Candace Pert, author of Molecules of Emotions, who discovered the opiate receptors while on his team) said that for many conditions, “such as migraine headaches or menstrual cramps, while something as mild as aspirin gives insufficient relief and opiates are too powerful, not to mention their potential for addiction. Cannabis might conceivably fulfill a useful role.”
Did You Know?
The categorization of this herbal medicine as a ‘drug’ – then a villainized illegal one – beginning in the late 1930s, is entangled with an overlay of anti-black and anti-Latino racism, the end of alcohol prohibition leading law enforcement to need a new target, which became weed smokers, and a massive anti-weed propaganda campaign, highlighted by the movie Reefer Madness. Its criminalization destroyed lives; in the first full year after the “Marihuana Tax Act” (1937), Black people were nearly three times more likely to be arrested for violating narcotic drug laws than Whites, and Mexicans were nearly nine times more likely to be arrested for the same charge. Additionally, many back-to-the lander hippies who were growing weed in places as varied as Vermont, North Carolina, and California, lost their homes, families, and freedom – well into the 2000s. Further, black people continue to be systemically being targeted and stigmatized by the “war on drugs.” According to the ACLU, “of the 8.2 million marijuana arrests between 2001 and 2010, 88% were for simply having marijuana,” and it's usually only a small amount.
Hormone Intelligence
Reclaim your power. Feel at home in your body. And be the force of nature you really are!
Limited Research, But a Lot of Evidence
Critics of Cannabis as a medicine are correct: there is far more anecdotal evidence for its effectiveness for menstrual pain than western scientific proof. This is largely because decades of illegal status severely limited scientific research, combined with the reality that women’s health – and particularly gynecologic pain – remains one of the least prioritized areas of scientific research, a problem women researchers are actively trying to address because it means that not only is our pain not effectively identified and addressed, but when we are treated, it’s with medications that have largely only been studied on men.
The illegal status – and stigma – associated with Cannabis use has also largely led women to keep their use under wraps to their doctors. Yet, when asked or surveyed, countless women swear by the relief it brings them. In 2015, researchers from the University of British Columbia asked a sample of 192 women if they had used Cannabis to relieve menstrual pain. Among these women, many had severe period pain as well as PMS and digestive symptoms; 88.5% said they had used marijuana (most had smoked or ingested it) and of these, 89.4% said it helped. It’s important to keep in mind, while Cannabis has been devalued by conventional medicine, consensus by a large number of individuals and historical use have validity and importance as forms of evidence.
How It Works
Cannabis is also backed by strong research into its pharmacology that strong supports clinical use.
The plant is rich in two cannabinoids, active chemical compounds amongst the over 100 compounds in this herb. The most well-known of these are tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is associated with psychoactive responses – ‘getting high’ – while CBD appears to modulate inflammation, muscle cramping, and mood.
The science behind Cannabis’ purported effectiveness in relieving period pain lies, in part, in the endocannabinoid system, (ECS). Discovered in the early 1990s, the ECS is a collection of cellular receptors that are found throughout the body, including the brain, the immune system, and abundantly in the female reproductive tract including the ovaries and uterus. Our own bodies produce a cannabinoid called anandamide (AEA), possibly in response to estrogen levels, which binds to these receptors and influences our moods, reproductive system immunity, inflammation, and likely a host of other functions still being explored. In binding to receptors in the reproductive system, cannabinoids from Cannabis, for which this system in our bodies is named, may lead to relief from period and pelvic pain, digestive system symptoms like gas and bloating, migraines or menstrual headaches, anxiety and irritability and other common PMS symptoms.
Although studies have not conclusively uncovered how Cannabis works to alleviate dysmenorrhea, it’s thought that:
- CBD and THC decrease pain sensation by targeting specific pain receptors in the body, TRPV1 and CB1 respectively, while also allowing more positive sensations to reach the brain.
- Both THC and CBD have anti-inflammatory effects. THC prevents macrophages, scavenger immune cells, from releasing inflammatory proteins called cytokines, while CBD, like NSAIDs, block COX-2, reducing inflammation. However, unlike NSAIDs which inhibit the COX-1 enzyme as well, leading to digestive symptoms in many people, CBD only inhibits COX-2, which doesn’t lead to digestive discomfort.
- CBD slows down electrical signaling to muscles, increasing muscle relaxation, and reducing cramping.
- CBD also appears to be effective in relieving anxiety, and may therefore also be helpful in PMS with anxiety for some women.
While clinical research on Cannabis and CBD on period pain is virtually non-existent, it’s worth noting that in 2017, when New York State was determining what conditions would qualify an individual for a Cannabis prescription, menstrual pain was on the list.
Is It Safe?
Overall, Cannabis is considered relatively low risk when used occasionally, as it would be for period pain. Smoking Cannabis and eating “edibles” that contain THC are more likely to produce side-effects, including acute anxiety, paranoia, focus and attention deficits, and decreased reflex time; however, the risk of serious or long-term adverse events is extremely low. Perhaps the most concerning risk, although rare, is that in a small subset of people, particularly teenagers with a specific genetic predisposition, THC has been known to precipitate psychosis. And of course, smoking anything is not ideal for your lungs.
CBD, taken as an extract, usually in the form of CBD oil, has an extremely low side effect profile. In 2018, the World Health Organization concluded in a review: “to date, there is no evidence of recreational use of CBD or any public health-related problems associated with the use of pure CBD,” and both CBD and Cannabis are generally safer than many of the medications available for the treatment of pain.
While it has not been associated with teratogenic effects, Cannabis use is generally not recommended for use in pregnancy, so unless for a medically supervised reason, discontinue use should you become pregnant.
Using Cannabis and CBD: Every Body is Different
Unfortunately, there’s no set of dosage guidelines nor one specific form of using Cannabis or CBD that has been shown to be more effective for dysmenorrhea. It just hasn’t been studied enough to reach any conclusions. Each of us has a unique threshold at which we might experience symptom relief, and also different levels of tolerance to the psychoactive effects of THC-containing products should you choose one of those. It can take a bit of gentle personal experimentation to determine whether Cannabis or CBD is right for you, which product, and at what dose.
A basic guideline: start low and go slow.
One additional guideline that I give my patients when it comes to treating period pain, including with NSAIDs, is don’t wait until the pain is miserable to treat; pre-empt it. Do the same with your holistic period pain prevention. If you typically start getting period pain a day or two before you start bleeding, start using calcium, magnesium, and some of the other natural remedies and approaches I mention here a few days ahead of time, and if needed, start using your chosen Cannabis or CBD product at the first twinge of discomfort.
What products should you consider? In my practice, I primarily recommend starting with products with the greatest safety and the least likelihood of immediate or longer-term side-effects, including:
Cannabis tincture: can be effective for pain relief, is taken in water so doesn’t require smoking anything, doesn’t cause psychoactive effects, and can be combined with other pain relieving, anti-inflammatory herbal tinctures, for example, a Cannabis-Cramp bark combination is a classic for menstrual pain relief. Tincture dose depends on the product you are using; commercially made products contain varying amounts of THC and CBD, so follow product instructions, start low, and go slow.
CBD oil: A good quality CBD oil product is usually made with an olive oil base, has zero to negligible THC so will not have a psychoactive effect, and can be conveniently taken by dropper with measurements on it to get accurate dosing, or in a capsule. I recommend my patients take the equivalent of 15 mg/day to start. But again, it’s best to start low, and go slow, to see how you personally respond.
CBD topical and suppository products: online companies, like Foria Wellness, specialize in high quality topicals and suppositories for women’s period and pelvic health.
I don’t recommend smoking unless other options just aren’t working for you. If you do find that this is the only way you get relief, keep it to just those few days of the month that you most need It, using only the smallest amount possible amount (for example, one or two tokes off of a thinly rolled joint). Purchase product from a Cannabis dispensary to ensure that it is a clean, good quality product, and ask for a low THC strain.
Hemp seeds: Another interesting approach for reducing the inflammation associated with causing period pain is the use of hemp seeds. The seeds, which do not contain cannabinoids, are rich in gamma-linolenic acid (GLA), in which women with PMS and dysmenorrhea have found to be low. In one study, a daily dose of 150 to 200 mg over 12 weeks greatly improved symptoms; this dose could be provided by a 5-mL daily dose of hemp seed oil.
Not a Panacea, But Worth a Try
Cannabis is not a panacea for all that ails us, as the Cannabis industry might have us believe. And it’s not a panacea for menstrual pain. Much more research is certainly warranted. It’s always important to look at all of your root causes, and treat those. But used safely and wisely, I do think Cannabis and CBD products may help many women with period pain to have a better experience of their menstrual cycles, and with fewer adverse effects than conventional medications.








